Throughout history, as humans spread across the world, infectious diseases were constant companions. Even in this modern era, outbreaks are nearly constant. History, after all, is our greatest teacher. And lest we forget, this article provides some glimpse into the past (https://www.history.com) and how the coronavirus pandemic will end is still being written.
The rise in global connections and interaction remains to be a driving force behind pandemics.
Let’s look at the five worst pandemics in the world and their take away messages – how it ended.
- Plague of Justinian – No One Left to Die

First appearing in Egypt, the Justinian plague spread through Palestine and the Byzantine Empire, and then throughout the Mediterranean.
The plague changed the course of the empire, squelching Emperor Justinian’s plans to bring the Roman Empire back together and casting massive economic struggle. It is also credited with creating an apocalyptic atmosphere that spurred the rapid spread of Christianity.
The Plague of Justinian arrived in Constantinople, the capital of the Byzantine Empire in 541 CE, carried over the Mediterranean Sea from Egypt. Egypt was a recently conquered land by the Emperor Justinian and was paying tribute to the emperor in grain. Plague-ridden fleas hitched a ride in rats that snacked on the grain.
The plague decimated Constantinople and spread like wildfire across all continents and killed an estimated 30-50 million people (around half the world’s population).
Today, it is more commonly known as Bubonic Plague brought about by the bacterium Yersinia pestis. But the plague would not end here as recurrences over the next 200 years would be recorded.
How it ended? We don’t know but the best guess is that majority of the people in the pandemic somehow survived because they had some form of immunity.
https://www.history.com/topics/middle-ages/pandemics-timeline
2. Black Death – The Invention of the Quarantine

Bubonic plague never really disappeared. Somewhere between 1347-1350 this disease which presents with enlarged lymphatic gland and chills and fever and later on gangrene of the extremities (toes, fingers, lips and tip of the nose) returned in Europe. During those years, there was still no treatment for this bacteria. And it was a painful way to die – with aches and extreme pain due to the decay and decomposition of the skin of the person while still alive. It claimed more than 200 million lives in just four years.
One-third of the world’s population was eliminated as this second large outbreak which started in Asia began moving west in caravans. It entered through Sicily, Italy in 1347 AD when plague sufferers arrived in the port of Messina and spread throughout Europe rapidly. Dead bodies became so prevalent that many remained rotting on the ground and created a constant stench in cities.
Because people still had no scientific understanding of the contagion, but knew that it had something to do with ‘proximity’, the Venetian-controlled port city of Ragusa decided to keep newly arrived sailors in isolation until they could prove they weren’t sick.
Trentino or 30-days forced isolation was implemented. But the Venetians were still seeing some cases in spite of the measure. They increased the forced isolation to 40 days or a quarantino – the origin of the word quarantine and the start of its practice in the Western world.
How did it end? The quarantine method was the beginning of a crude but effective way of isolating sick patients until they were no longer infectious – survived or died – from the disease.
https://www.history.com/topics/middle-ages/pandemics-timeline
3. The Great Plague of London – Sealing Up the Sick

In reality, London never really caught a break after the Black Death, with the plague resurfacing every 20 years from 1348 to 1665 – 40 outbreaks in 300 years.
In the early 1500s, England imposed the first laws to separate and isolate the sick. Homes stricken by plague were marked with a bale of hay strung to a pole outside. If someone among your family members was infected, you had to carry a while pole when you went out in public.
The bubonic plague led to a decimation of twenty percent of London’s population. With increasing human death tolls, mass graves appeared. To stifle the transmission of the fleas, hundreds of thousands of cats and dogs were slaughtered as the possible cause. The worst of the outbreak tapered off in the fall of 1666, after killing more than 100,000 Londoners in just seven months.
All public entertainment was banned and victims were forcibly shut into their homes (isolation) to prevent the spread of the disease. Red crosses were painted on their doors along with a please for forgiveness: “Lord have mercy upon us.”
How did it end? As cruel as it was to shut up the sick in their homes and bury the dead in mass graves, it may have been the only way to bring the last great plague outbreak to an end.
https://www.history.com/news/pandemics-end-plague-cholera-black-death-smallpox
4. Smallpox – From biological warfare to vaccine development

While smallpox was believed to have appeared around 10,000 BC, at the time of the first agricultural settlements in northeastern Africa, it is likely that it spread to India by means of ancient Egyptian merchants.
It has been reported in ancient Asian cultures as early as 1122 BC in China and is mentioned in ancient Sanskrit texts of India.
It was introduced to Europe between the 5th and 7th centuries and was frequently an epidemic during the Middle Ages. The disease greatly affected the development of Western civilization. The first stages of the decline of the Roman Empire (AD 108) coincided with a large-scale epidemic: the plague of Antonine, which accounted for the deaths of almost 7 million people. The Arab expansion, the Crusades, and the discovery fo the West Indies all contributed to the spread of the disease.
Unknown in the New World (meaning these people had zero immunity) , smallpox was introduced by the Spanish and Portuguese conquistadors. The disease decimated the local population and was instrumental in the fall of the empires of the Aztecs and the Incas. On the eastern coast of North America, the disease was introduced by early settlers leading to a decline in native population.
The discovery of the devastating effects of smallpox was the birth of “biological warfare”. During the French-Indian war (1754-1767), Sir Jeffrey Amherst, the commander of the British forces in North America, suggested the deliberate use of smallpox to diminish the American Indian population hostile to the British.
Another factor that contributed to smallpox in the Americas was the slave trade because many slaves came from regions in Africa where smallpox was endemic.
Smallpox or variola affected all levels of society. In Europe during the 18th century, 400,000 people died annually of smallpox and one third of survivors went blind. Otherwise called the “speckled monster” had devastating sequelae. The case-fatality rates varied between 20% – 60% and left most survivors with disfiguring scars. Among infants, the case-fatality rate was even higher – 80% in London and 98% in Berlin during the late 1800s.
Survivors of smallpox became immune to the disease and ended up tending to those subsequently became affected by it. Many herbal remedies were concocted, but the most successful way of combatting smallpox before vaccination was discovered was inoculation.
Inoculation involved the subcutaneous instillation of smallpox virus into people who had no immunity to it. The inoculator used a lancet wet with fresh matter from a ripe pustule of someone who suffered from smallpox. The material was the introduced subcutaneously on the arms or legs of the non-immune person. And this was not without its attendant risks – disseminated smallpox, spread of other individuals and transmission of diseases (syphilis was predominant during this era). This gave birth to the term variolation.
In Europe, where the medical profession was relatively organized, the new methods of variolation became known quickly among physicians. Since there was a demand for protection against smallpox, doctors began the variolation procedure on a massive scale. This was, however, not without adverse effects as 2% to 3% of variolated persons died from the disease, became the source of another epidemic, or suffered from other diseases transmitted by the procedure itself. Nevertheless, this became popular among both the aristocrats and common people in Europe and the case-fatality rate associated with variolation was 10 times lower than that associated with naturally occurring smallpox.
The long history of variolation had spread to North America and during the great epidemic of 1721, almost half of Boston’s 12,000 citizens contracted smallpox. The fatality rate for naturally contracted disease was 14%, whereas patients variolated by Boylston and Mather (Rev. Cotton Matter and Dr. Zabdiel Boylston) reported a mortality rate of only 2%. This was the first time that comparative analysis was used to evaluate a medical procedure.
As variolation became an acceptable method of prevention of the disease, it was rapidly adopted in Europe. In spite of the skepticism from British physicians after Mather’s success, it was subsequently adopted in England and spread from there throughout Western Europe.
In 1757, an 8-year old boy was inoculated with smallpox in Gloucester – one of thousands of children inoculated that year in England. The procedure was effective, as the boy developed a mild case of smallpox and became immune to the disease.
His name – Edward Jenner.
How did it end? Dr. Edward Jenner is credited for the discovery of the smallpox vaccine. Jenner’s interest in the protective effects of cowpox began during his apprenticeship with George Harwicke. For many years, he had heard the tales that dairymaids were protected from smallpox naturally after having suffered from cowpox. He concluded that cowpox not only protected against smallpox but also could be transmitted from one person to another as a deliberate mechanism of protection. In May 1796, Edward Jenner found a young dairymaid, Sarah Nelms, who had fresh cowpox lesions on her hands and arms. Using the matter from Nelms’ lesions, he inoculated an 8-year old boy, James Phipps. The boy developed mild fever and a discomfort in the axillae. Nine days after the procedure he felt cold, lost his appetite but on the next day he was much better. In July 1796, Jenner inoculated the boy again, this time using matter from a fresh smallpox lesion. No disease developed and Jenner concluded that protection was complete.
While the scientific community was skeptical with this discovery of Jenner (it was initially rejected by many physicians and scientists), those that did introduced the vaccine (as the term vaccination – latin word for cow is vacca and cowpox is vaccinia, Jenner decided to call this new procedure vaccination) among their patients and those willing to get protected against the disease.
Although Edward Jenner received worldwide recognition and many honors, he made no attempt to enrich himself through his discovery. He actually devoted so much time to the cause of vaccination that his private practice and personal affairs suffered severely. However, he not only received honors but also found himself subjected to attacks and ridicule. Despite all this, he continued his work of behalf of the vaccination program and eventually, vaccination replaced variolation, which became prohibited in England in 1840.
In the 1950s a number of control measures were implemented, and smallpox was eradicated in many areas in Europe and North America. The process of worldwide eradication of smallpox was set in motion when the World Health Assembly received a report in 1958 of the catastrophic consequences of smallpox in 63 countries. In 1967, a global campaign was begun under the guardianship of the World Health Organization and finally succeeded the eradication of smallpox in 1977.
On May 8, 1980, the world never saw a case of smallpox ever again. It was and still is the only virus ever eradicated in the world with the use of a vaccine.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1200696/
5. Cholera – A Victory for Public Health Research

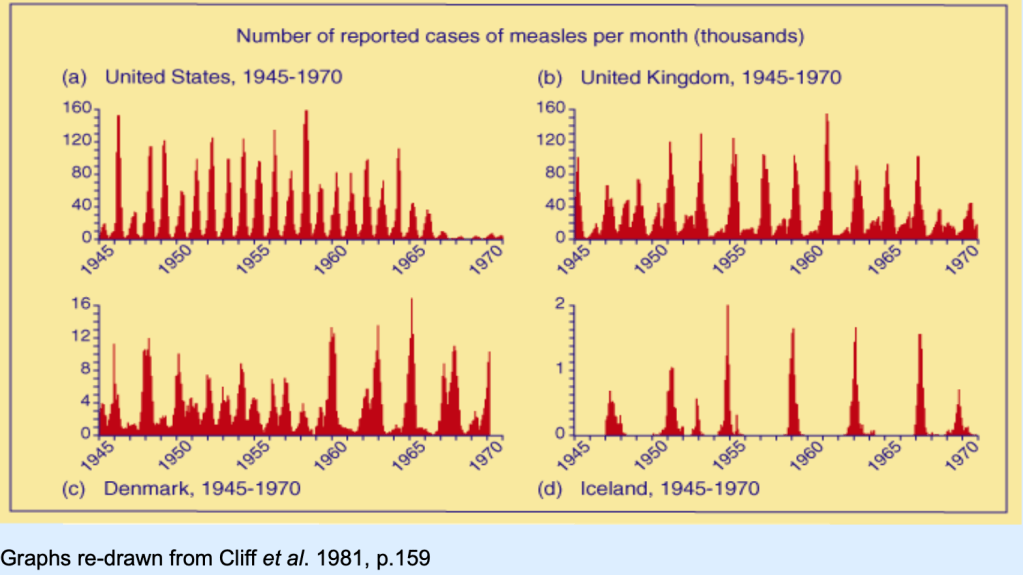
During the 19th century, cholera spread across the world from its original reservoir in the Ganges delta in India. Six subsequent pandemics killed millions of people across all continents. The seventh and last pandemic started in South Asia in 1961, and reached Africa in 1971 and the Americas in 1991. Cholera is now endemic in many countries.
The prevailing scientific theory of the day said that the disease was spread by foul air known as “miasma”. It was third pandemic (1852-1859) that was the deadliest. It devastated Asia, Europe, North America and Africa, killing 23,000 people in Great Britain alone in 1854, the worst single year of cholera.
In that year, British physician John Snow, considered one of the fathers of modern epidemiology, carefully mapped cholera cases in the Soho area of London, allowing him to identify the source of the disease in the area – CONTAMINATED WATER FROM A PUBLIC WELL PUMP.
Snow convinced officials to remove the pump handle so that people could not drink the well, immediately dropping the cholera cases in the area.
How did it end? The birth of the sleuthing world of epidemiology and public health addressed measures at improved water supplies, public health and sanitation and quarantine.
Today, vaccination and antimicrobial treatment had decreased the morbidity and mortality of cholera, although there are still outbreaks worldwide (in 2017 in Somalia and Yemen) and until health and sanitation remains a problem in poorer countries in the world, this disease will remain in our midst.
https://www.who.int/news-room/fact-sheets/detail/cholera; https://www.history.com/topics/inventions/history-of-cholera
The list of pandemics enumerated is not exhaustive.
And neither is it exclusive. Which means that some pandemics are worse because of ongoing diseases and timeline overlap from one disease to another.
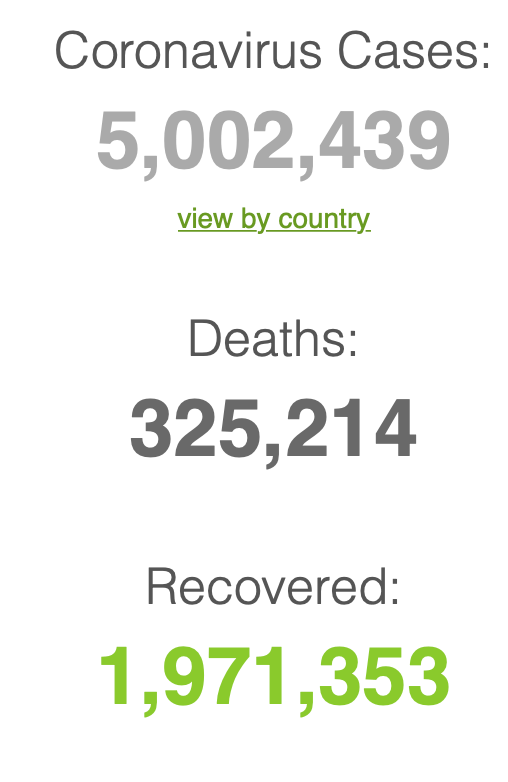
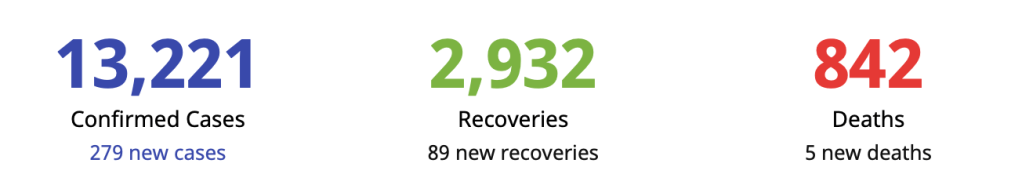
As the world goes through an unknown, formidable virus in modern-day 21st century, it is important to recall the lessons of various history of pandemics. There are take away lessons here and we need to do our share in making sure that human lives do not end up as mere statistics of history.
How will the coronavirus pandemic end? Only history will tell its story.