The world changed overnight with the COVID-19 pandemic.
So did our lives.
Masks became part of the new normal. Travel – whether by land, air or sea – unless essential for work was parked. Borders both locally and internationally were closed. The economy broke its back as mobility became compromised. What stood out was how the pandemic served as the great divide between rich and poor countries, rich and poor people. Inequity became more glaring during the past one and half years.
The world needed to live differently. At an age of technological, digital and economic advances, the new normal was mentally and emotionally challenging.
In the Philippines, schools never reopened face-to-face. The irony here is that while many other municipalities and cities in the 7,641 islands in the archipelago had very few COVID-19 cases, the whole education system had a one strike policy – shut it down. And for a country whose internet speed and regular stream of energy supply is wanting, this was a misguided decision of government. The disruption in our normal daily lives was more apparent among the frontline healthcare workers and the daily wage earners in society. Lockdowns became the primary measures at curtailing the spread of the virus.
The year 2020 was traumatic to everyone. When the first surge came, the health workers were overwhelmed. It was a time when we scrambled searching for a cure while some friends, families and colleagues who got infected died. Several drugs were repurposed as we waited on the sidelines for vaccines. Using new and old platforms, science was on a mad dash to developing vaccines to stem the pandemic’s growth.
Towards the end of 2020, some manufacturers were ready to roll out vaccines. The COVID-19 vaccines were approved for Emergency Use Authorization (EUA) in less than a year. The quickest ever. The entry of a new platform using mRNA technology provided the first ray of light at the end of the deep dark tunnel. Other vaccine platforms – non-replicating viral vector (Astra-Zeneca Oxford, Sputnik V, Janssen), inactivated virus (Sinovac, Sinopharm), and subunit protein (Novavax) – rolled out their clinical trial results one after the other. To date, there are more than 80 vaccines in development at various phases of clinical trials. A testimony of humanity working together towards that light.
While vaccines are now available, the glaring prejudice for countries or continents that have more resources compared to poor nations has become more apparent than ever. Israel, the UK, the US are examples of model and wealthy nations that have managed to address the pandemic with the abundance of vaccines available to them. The saying “beggars can’t be choosers” is strikingly more vivid now, with developing and third world countries like ours having to literally beg for that shot of hope.
With vaccines coming in dribbles for now, how the available COVID-19 vaccines at our disposal are being rolled out, is even a challenging one.
The first challenge is the war against vaccine hesitancy.
Vaccine acceptance was never a problem in the Philippines. Until the political story behind Dengvaxia came along. After the Dengvaxia fiasco – with theatrics and drama at the level of congress and the senate – rebuilding vaccine confidence became an uphill battle. Social media and reckless sensational journalism heightened the misinformation and false information campaign. While it is true that Dengvaxia was prematurely rolled out as a public health program by the past administration, the vaccine was vilified and stripped of its potential use among those who may benefit from a vaccine against dengue. During the deliberations in congress and the senate, science was thrown under the bus. At the end of the Dengvaxia debacle, science and research were lost in translation. The wrong people were crucified. And public trust in vaccines were lost overnight.
The Dengvaxia story would be one that would be the first straw to severely affect preventive healthcare in the country. Parents refused to have their children immunized. An outbreak of measles ensued. Followed by polio. Then dengue. Sadly, the more vulnerable sectors of society – classes C, D and E – were the most affected.
Then came the COVID-19 pandemic. And while the world was not prepared for a pandemic of this magnitude, the ghost of Dengvaxia past was still fresh in the minds of the Filipino people. Deeply ingrained even as vaccines against COVID-19 started to arrive and roll out, that ghost would haunt our vaccination efforts.
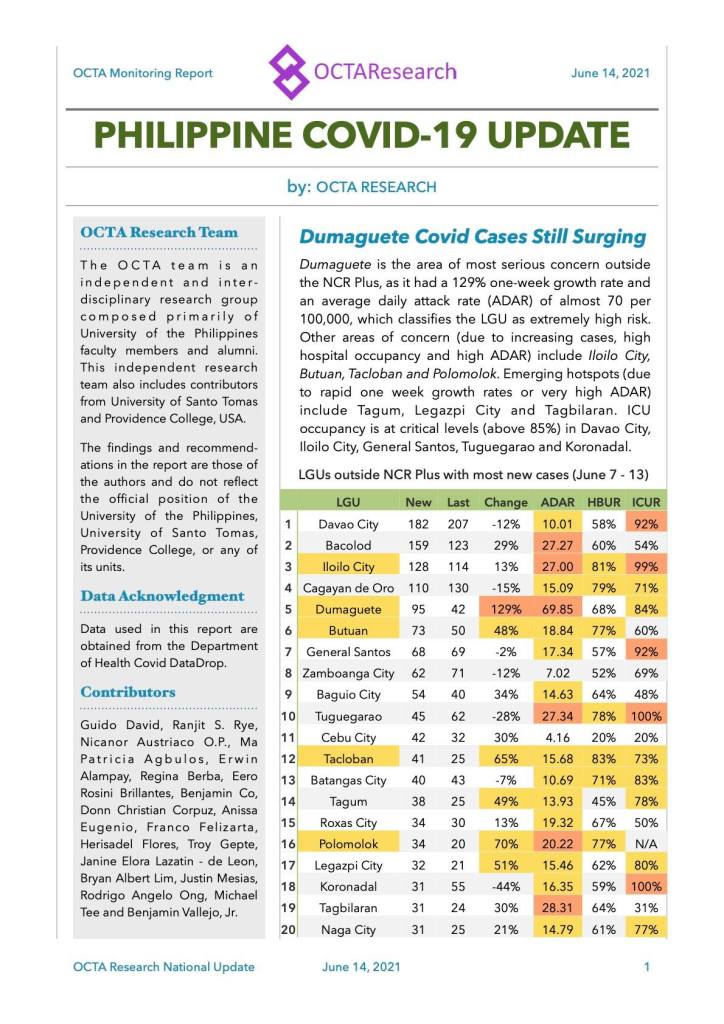
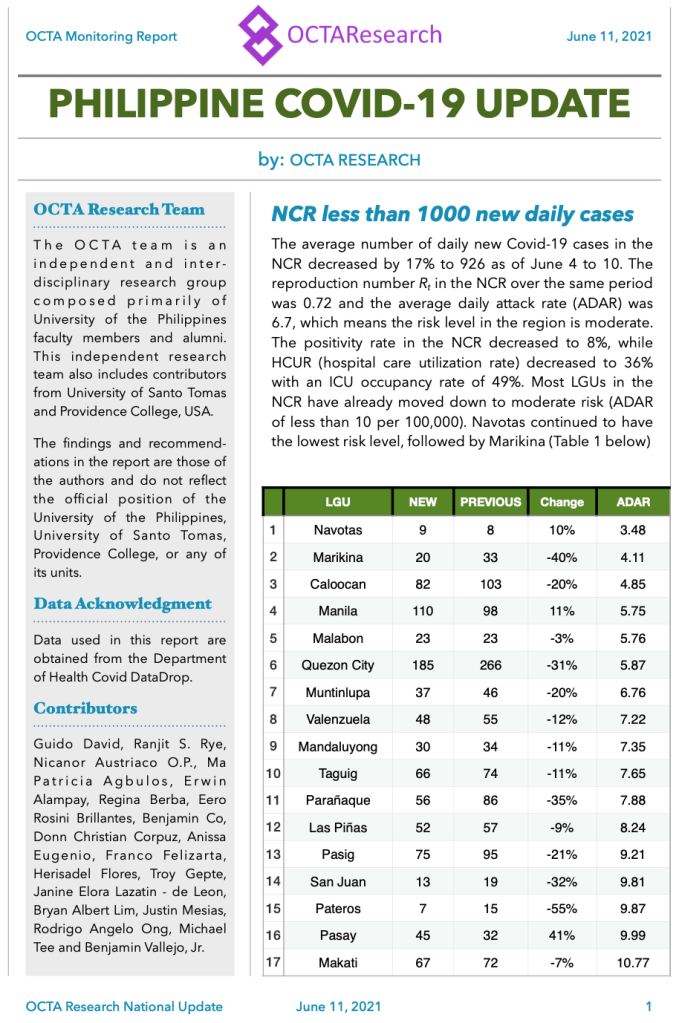
In several early surveys done by independent organizations (SWS, OCTA RESEARCH, Pulse Asia), vaccine acceptance against COVID-19 was initially very low. The brand also mattered. There was distrust from those made in China and Russia. The tragedy created by the Dengvaxia story created a wedge so deep with fear that many people were more than willing to risk infections rather than getting injections.
As the title in a Nature article would say, “six months and 1.7 billion doses later“, where are we in the effort to address the pandemic?
That leads us to second challenge – restoring vaccine confidence.
On December 8, 2020, at 630AM, Margaret Keenan, a 90 year old British woman became the first person in the world to receive a COVID-19 vaccine (Pfizer-BioNTech) as a mass vaccination effort at University Hospital in Coventry. On April 22, 2021, Maggie was interviewed once more, and called the global mass vaccination rollout as “incredible”. She has turned 91 since, and continues to be the poster woman who took the first jab during the pandemic.
Without a doubt, the vaccines work. Their efficacies vary from clinical trial settings and since their roll out in the real world, much of the news continues to be positive on how well the vaccines perform in general settings.
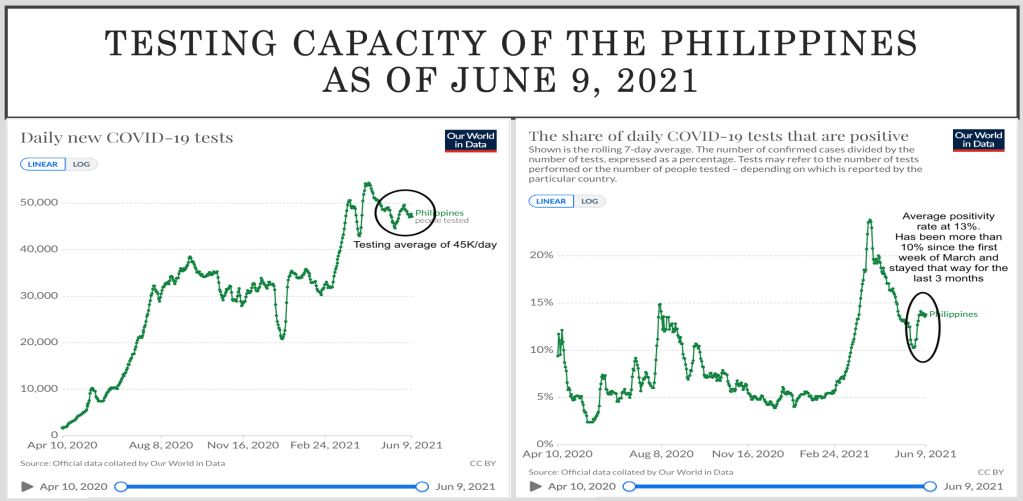
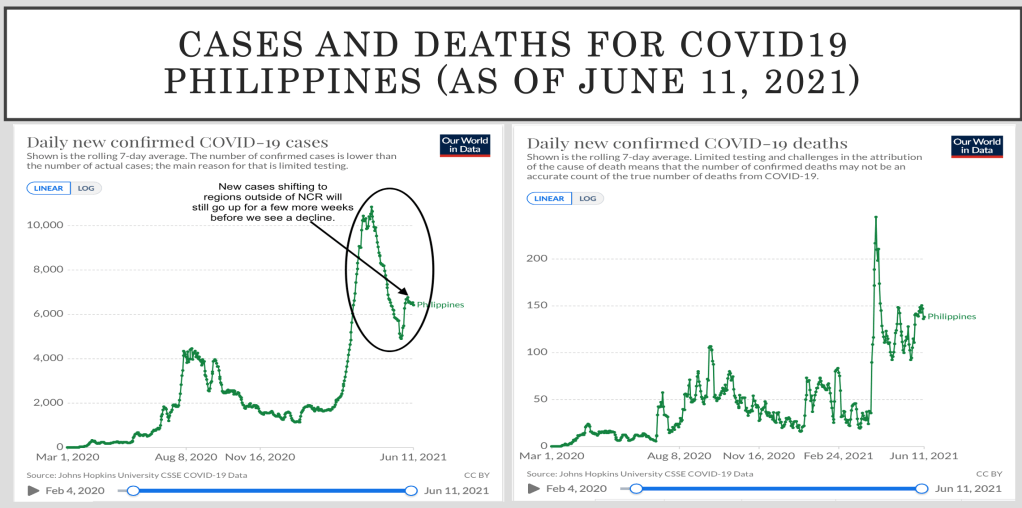
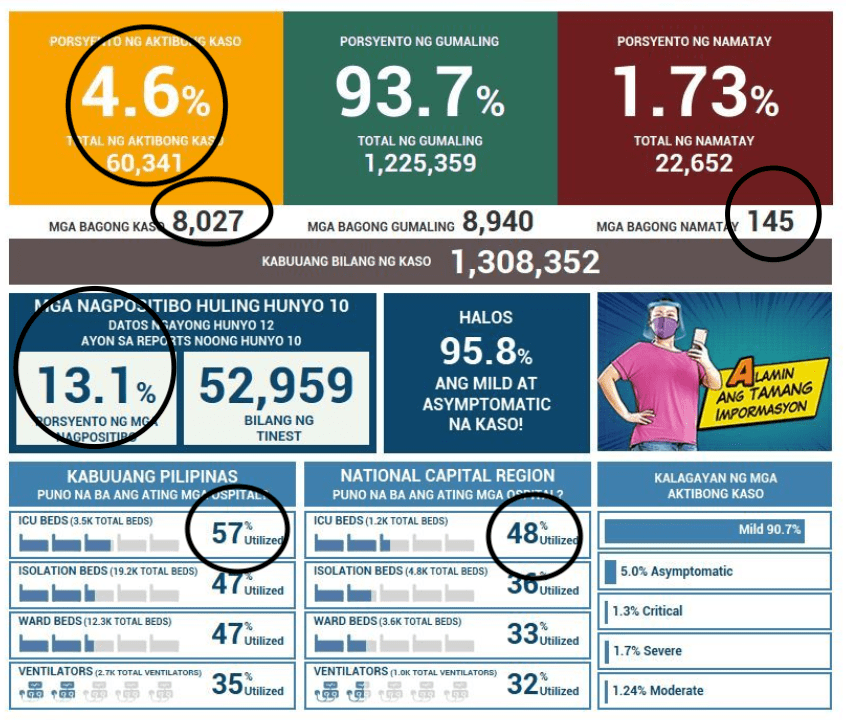
As a general rule, the ideal time to roll out a vaccine program is when the cases are low. If you wait to do this when the cases are running through the roof then one will need to combine this with extensive limitation of mobility (e.g., lockdowns) to give time for the vaccines to provide immunologic responses to those that get the shot. Starving the virus entails stemming the transmission from person to person either by limiting movement of individuals in society or having them vaccinated.
Restoring vaccine confidence will entail a lot more work than just providing lip service. The communication strategy should be one that appeals to the concerns (safety and suitability) of the masses. The major question that is asked – IS IT SAFE?
We will need more than just one Keenan out there to show the world that the vaccines work and are safe. With an unparalleled speed in the roll out of a vaccine, surveillance systems must be put in place to watch out for adverse events, record them, and identify if there is a link between the vaccine and that reported side effect. So far, the concerns include clotting syndrome with vaccines from an adenovirus platform, anaphylactic reactions after immunization, and lately, the possible link of myocarditis (heart inflammation) among those 16-19 years old who received Pfizer-BioNTech vaccine. The debate on the safety of these vaccines was enough to dampen public confidence in them.
What level of safety is acceptable?
Even the food we eat, or the air we breath or the water we drink have potential risks. Over the counter multivitamins or supplements have different manufacturing standards and can pose harm even to those who perceive that they are absolutely safe.
There is no answer that will guarantee with absolute certainty that the vaccines are 100% safe. Some side effects will occur. Whether it is local or systemic, majority will be mild, tolerable, and inconsequential. To date, the number of people who have developed adverse events to the COVID-19 vaccines available as EUA are far fewer than the 1.7 billion doses that have been administered. Definitely, a case where the benefits far outweigh the risks.
The final challenge is equity at a time of scarcity.
When the COVID-19 vaccines began its initial roll out in the Philippines, the healthcare workers were the priority. Not many wanted to get the first jab. It was a disappointment that instead of an mRNA that arrived, a vaccine made in China came. But we rolled up our sleeves and took the jab anyway.
A study published in the American Journal of Preventive Medicine on “The Benefits of Vaccinating With the First Available COVID-19 Coronavirus Vaccine” by Bartsch et al. last January 18, 2021 argues why “during a pandemic, there are many situations in which the first available vaccines that may not have as high effectiveness as vaccines that are still under development or vaccines that are not yet ready for distribution” raise the question of whether it is better to go with what is available now or wait. After all, it is a valid concern by all.
The authors of that study developed a computational model representing the spread of COVID-19 and vaccines with different efficacies (either to prevent infection or reduce severity of disease), vaccination timing and the clinical and economic value of vaccination.
That study showed that, using the United States of America population as computational model, “if a vaccine with 50% efficacy in preventing infection becomes available when 10% of the population has already been infected, waiting until 40% of the population are infected for a vaccine with 80% efficacy in preventing infection results in 15.6 million additional cases and 1.5 million additional infections, costing $20.6 billion more in direct medical costs and $12.4 billion more in productivity loses.”
Clearly, there are few situations where it is even worth foregoing the first available COVID-19 vaccine in favor of one that becomes available later on during an ongoing pandemic, even if the one we are waiting for has a substantially higher efficacy.
At at time when the vaccines that are arriving are coming in trickles, let us remember that the ultimate aim of vaccination is creating herd protection. This can only be achieved when majority of us are immunized, regardless of the vaccine platform. There are many factors that affect response to a vaccine. We need to keep in mind that the best one is the one in our arm. And when we get more arms getting the shot, then it becomes more difficult for the virus to transfer from a person who is protected to an unprotected individual.
But there is a need to equitably distribute the available vaccines across all classes of society.
The systems that allow people to get vaccinated should not rely on technology alone because people in classes C, D and E will most likely not have the same means and resources as those in class A and B. Being able to register for vaccination using technology is unjust and inequitable. It is prejudicial to the poor who will always be left behind. As a consequence, the effect of being noninclusive in a society that treats them differently, pandemic or not, is a challenge for every local government.
In spite of the vaccine roll out, every nation cannot fully depend on lockdown measures and vaccines as the only strategy at addressing the pandemic. Economies will suffer and those who have the least will have a longer journey through the tunnel. Unless a feasible exit plan is laid out.
At the end of the day, the impact of the pandemic will continue to be felt until every eligible person from high-, middle- or low-income countries can be immunized.